Biomaterial developed at Rensselaer shows promise as spinal cord injury treatment
March 19, 2021
A novel form of polymerized estrogen developed at Rensselaer Polytechnic Institute can provide neuroprotection when implanted at the site of a spinal cord injury — preventing further damage. This promising result, found in a preclinical model, was recently published in ACS Chemical Neuroscience, and it lays the groundwork for further advancement of this new biomaterial.
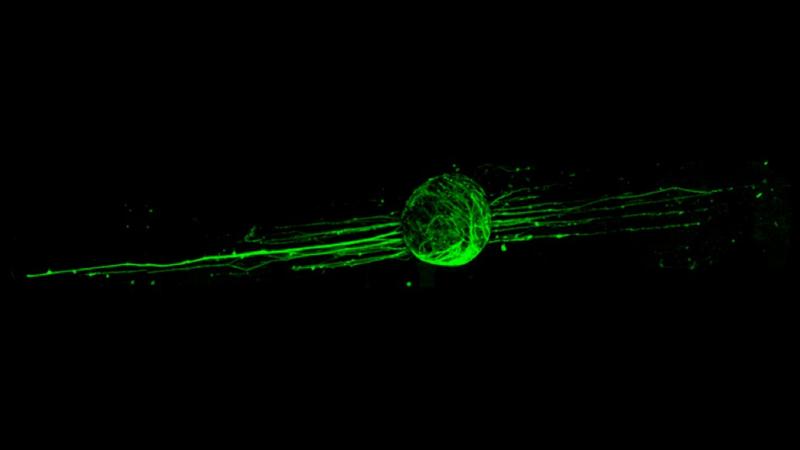
“What we saw that gives us hope is more neuroprotection, meaning we saw more spared neurons and more spared axons in the tissue,” said Ryan Gilbert, a professor of biomedical engineering at Rensselaer, and co-author on this paper. “We believe that the estrogen released from our biomaterial design is providing a neuroprotective response.”
After a spinal cord injury, the body’s inflammatory response can cause further damage to nervous system cells — like a loss of neurons and axons — even beyond the site of initial injury. A solution that could prevent additional deterioration, or even promote regeneration over time, could be a paradigm shift in treatment. Estrogen is a natural hormone produced within the body. When polymerized, it shows promise as a source of neuroprotection following a spinal cord injury.
Gilbert, a member of the Center for Biotechnology and Interdisciplinary Studies at Rensselaer, collaborated with Edmund Palermo, an associate professor of materials science and engineering at Rensselaer, to design this polymer. The preclinical aspect was initiated by Manoj Gottipati, a Rensselaer research associate, currently working in the laboratory of Phillip Popovich, professor and chair of the Department of Neuroscience at The Ohio State University. At Ohio State, Gottipati worked with Zhen Guan from the Center for Brain and Spinal Cord Repair to test the polymerized estrogen film. The researchers observed enhanced neuroprotection in a preclinical mouse model that had the implanted polymerized estrogen when compared to models that did not receive this treatment.
The polymer itself is entirely made of estrogen, which is released slowly within the body over time as water reactions break down the bonds that hold the polymer chain together, making it a unique and promising therapeutic approach.
“Since the drug molecule is enchained in every repeating unit of the long chain, it contains a very high drug load compared to conventional delivery approaches,” said Palermo, who is also co-author on this paper and a member of the Rensselaer Center for Materials, Devices, and Integrated Systems.
According to Palermo, the polymer studied in this research is one of a number of candidates the researchers will continue to investigate as they work to find the optimal release rate for enhanced neuroprotection. Finely tuning hydrophobicity, mechanical properties, and hydrolysis rates could all make a difference in critical aspects of its performance, such as how quickly the polymer releases estrogen within the body.
“All of those factors will play a role in the complex cascade of biochemical and biophysical events that occur during the course of the body’s reaction to spinal cord injury,” Palermo said.
As the team continues to modify this biomaterial, what researchers develop could have implications beyond spinal cord injury therapeutics.
“I would say that this approach could be used for any sort of central nervous system injury, from spinal cord to brain injury,” Gilbert said. “Anything where we could inject or place it near the injury site and have that therapy be released for an extended duration.”